Cervical cancer screening
Cervical cancer screening can prevent cancer!
Can cervical cancer screening actually prevent cancer? Yes, because cervical cancer is caused by a long-lasting HPV infection, and it takes years for precancerous lesions to develop and eventually become cervical cancer. This article explains how cervical cancer can be detected before it even develops.
How does cervical cancer screening work?
Cervical cancer screening is an integral part of the normal check-up at the gynecologist. Many women don’t know the details of this examination. If you feel the same way, you are not alone. As the costs for cervical cancer screening are covered by health insurance, you have never held the bill in your hand.
Most women are familiar with the smear test when visiting the gynecologist. The woman sits down on the examination chair and the gynecologist inserts a speculum into the vagina to gently open it. Then, she inserts a kind of brush and strokes it over the cervix. Cells stick to the brush, and these cell samples are sent to a laboratory for examination.
Depending on the woman’s age, the cervical cancer screening program includes a Pap test or a combination of Pap and HPV tests. A Pap test examines the smear sample for cell changes, while an HPV test examines whether there is an infection with human papilloma viruses.
The regulated cervical cancer screening program
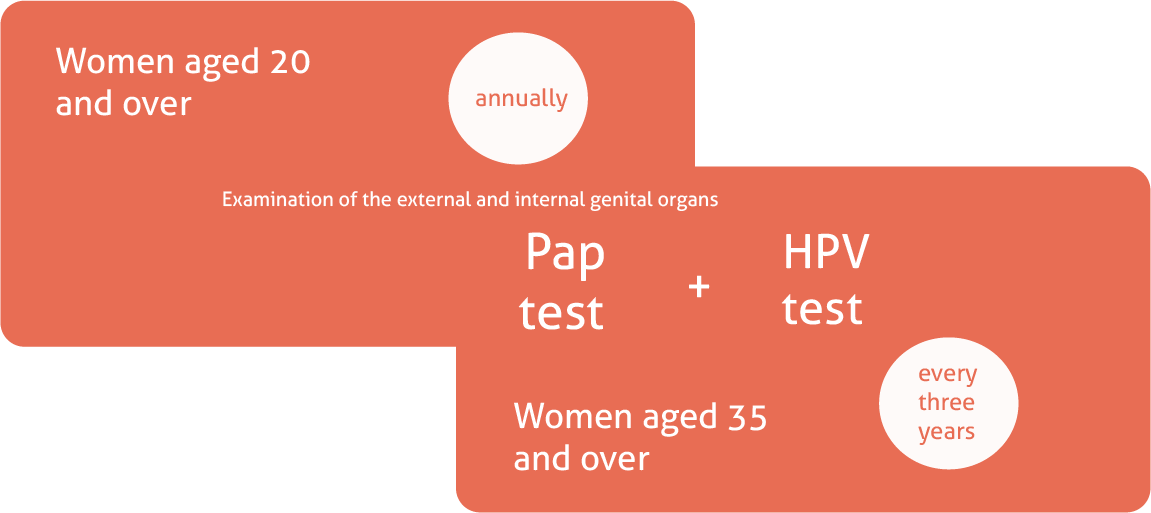
Cervical cancer screening in Germany was restructured in 2020. The main changes were that age groups were introduced and screening intervals were adjusted accordingly. In addition, the HPV test was added alongside the Pap test for certain age groups.
Women between the ages of 20 and 34 can have a Pap smear once a year. This is a cytological examination in which the gynecologist takes a smear from the cervix using a kind of brush. The cells which remain on this swab are then examined in a laboratory. It is particularly common for cell changes to be detected in younger individuals. In most cases, however, they disappear. Nevertheless, an abnormal result must either be monitored or followed up with further examinations. The type of examinations will depend on the result of the Pap test.
From the age of 35, women receive a combined examination consisting of a Pap test and an HPV test paid for by their health insurance every three years. The HPV test examines the cervical smear for human papillomaviruses (HPV), which are known to cause cervical cancer. Here too, the result determines whether further examinations are necessary. However, an HPV infection only indicates an increased risk of developing cervical cancer. This means that a positive HPV test is not yet a cancer diagnosis.
Why is a Pap smear only carried out every three years?
If an annual Pap test is recommended for younger women and is paid for by the health insurance companies, the question naturally arises as to why women over the age of 35 only have a Pap smear every three years. It was precisely this change which led to uncertainty when the new programme for the early detection of cervical cancer was introduced.
The answer lies in the development of cervical cancer. Human papillomaviruses, HPV for short, can cause cell changes on the cervix that develop into cervical cancer. However, this only happens with a long-term infection. In addition, almost everyone is infected with HPV at least once in their lifetime. These viruses are transmitted sexually and condoms do not protect against an HPV infection. In most cases, the infection is so harmless that it’s unnoticeable. Only in very few cases does cervical cancer develop.
HPV infections tend to be more common in younger individuals due to a higher rate of sexual activity and changing sexual partners. For this reason, younger women go for an annual Pap test, because an HPV test would only sound an unnecessary false alarm.
Women aged 35 and over are tested every three years not only with the Pap test, but also with the HPV test. An HPV infection persists for several years before it triggers cell changes. So the conclusion is: If the woman has been tested HPV-negative, cervical cancer is not expected in the next three years. No HPV infection means cervical cancer cannot develop.
What tests are carried out for cervical cancer screening?
There are two tests that are used for cervical cancer screening: The Pap test and the HPV test:
Pap test:
For the Pap test, a gynecologist takes a swab from the mucous membrane of the cervix. To do this, they insert an instrument that looks like a long cotton bud or brush. The sample is then sent to a laboratory and examined under a microscope for cell changes.
HPV test
For the HPV test, the gynecologist also swabs a sample from the cervical mucosa. Women do not normally notice the difference between Pap and HPV tests. A laboratory then determines whether human papillomaviruses are present.
Tfhe GynTect® test
Quick verification
in case of suspected
cervical cancer
What to do after an abnormal cervical cancer screening result?
If the gynecologist’s office calls because the result of the cervical cancer screening was abnormal, this usually triggers a shock. What should you do now? Take a deep breath, ask your doctor all the questions that come to mind and remember: abnormalities in cervical cancer screening are not a diagnosis. They are only indications that should be followed up in further examinations.
After an abnormal cervical cancer screening result next steps depend on various factors including whether the woman is HPV-positive or negative, the Pap test findings, and the patient’s medical history.
Since cell changes can regress on their own, Pap and HPV tests are often repeated after a short period of time. The doctor may also recommend a vaginal endoscopy, also known as a colposcopy, which involves taking a closer look at the cervix using a special microscope. The affected women often have to make an appointment at a so-called dysplasia consultation in a specialized practice for a colposcopy, because not every gynaecologist’s practice offers this examination.
Conclusion
Yes, cervical cancer screening can prevent cancer. The cause is known to be an infection with certain human papilloma viruses (HPV). If the HPV infection becomes chronic, i.e. lasts for years, the cells on the cervix can change, become precancerous and eventually develop into cervical cancer.
So, if you go for regular cervical cancer screenings, there is a good chance that changes will be detected before they become malignant.
Order GynTect®
Contact us, to get GynTect®
On request, you will receive a free smear test kit, which is accompanied by a treatment contract. Only when we have received the swab sample together with the signed examination request in the laboratory do you undertake to pay the costs of 150 euros.
Do you have any further questions? Please use the contact options provided.
oncgnostics GmbH
Löbstedter Str. 41
07749 Jena
Germany
Contact us if you have any further questions:
Picture credits
- Titelbild: fizkes / Shutterstock.com
- Grafik: oncgnostics GmbH